What is a Culture of Health?
Most people tend to think about health only when they don't have it. They also usually think of health in terms of disease and treatment by a healthcare provider. For decades, this is how most of our society looked at health. We ignore it until something goes wrong, then we go to the doctor to get it fixed. There are two main problems with looking at health in this way. One is that it doesn't work very well and the other is that it is an incredibly expensive way to manage health.
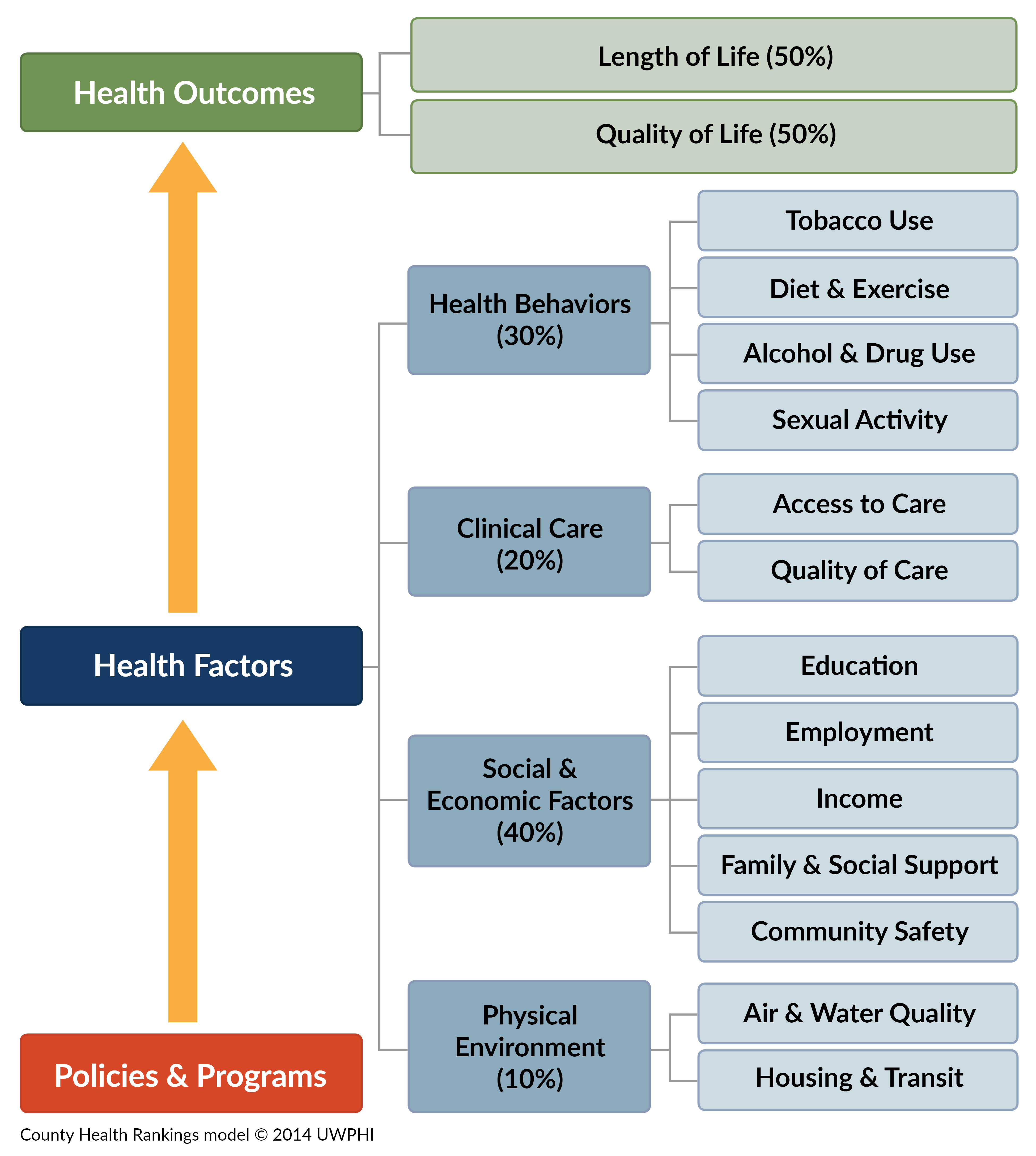
In the model above, clinical care, which is what we mostly think of as "health", accounts for only about 20% of the factors that contribute to a person's health. The other 80% are what are called "social determinants of health. 10% is attributable to how a person lives, if they have access to transportation and the environmental pollutants they are exposed to. 30% is in the choices people make--what they eat, do they exercise, do they smoke, do they engage in risky behaviors, and so forth. The remaining 40% is due to socioeconomic factors like income level, education level, whether they are employed and at what job they are employed, the neighbor where they live, their support networks, etc. These various factors can be changed through good policies and programs to achieve better outcomes, which can be defined as how long a person lives and how healthy they are and what quality of life they enjoy.
The idea of a Culture of Health is that, to truly improve individual and community health, we need to work on improving ALL of these factors that impact health. We need to change the way we look at the health of ourselves, our families, our neighborhoods and our communities. We need to make better choices. We need to work to make sure people have better options for healthy food and housing, opportunities for fitness, stress relief, behavioral health care and many other things that are all related.
You can read more about what a Culture of Health is at the Robert Wood Johnson Foundation web site https://www.rwjf.org/en/cultureofhealth.html . The Robert Wood Johnson Foundation is the world's largest philanthropic organization devoted to health. They developed the idea of the Culture of Health in order to make sure the money they were spending was actually making people's lives better.
Part of the RWJF Culture of Health movement is what is called the Culture of Health Leaders (CoHL) Program. You can read about it on the site, but the gist of it is that they wanted to bring together a group of people who are already leaders working in all different areas related to health--business, healthcare, community services, education, housing, nutrition and so on--and then help them learn how to become better, and more effective leaders working for the health of their communities. I was selected to be part of the first cohort of the CoHL program. It's a three-year program, and we have just graduated. I learned an amazing amount about community organization, leadership techniques, public health issues and more, but mostly, I learned about people and how different people experience the world differently. Health and healthcare mean very different things to different people. Here's an interview about some of my experiences in the Culture of Health Leaders Program.
Our cohort, comprised of 40 people from all over the country, put together an infographic of our definition of a Culture of Health.
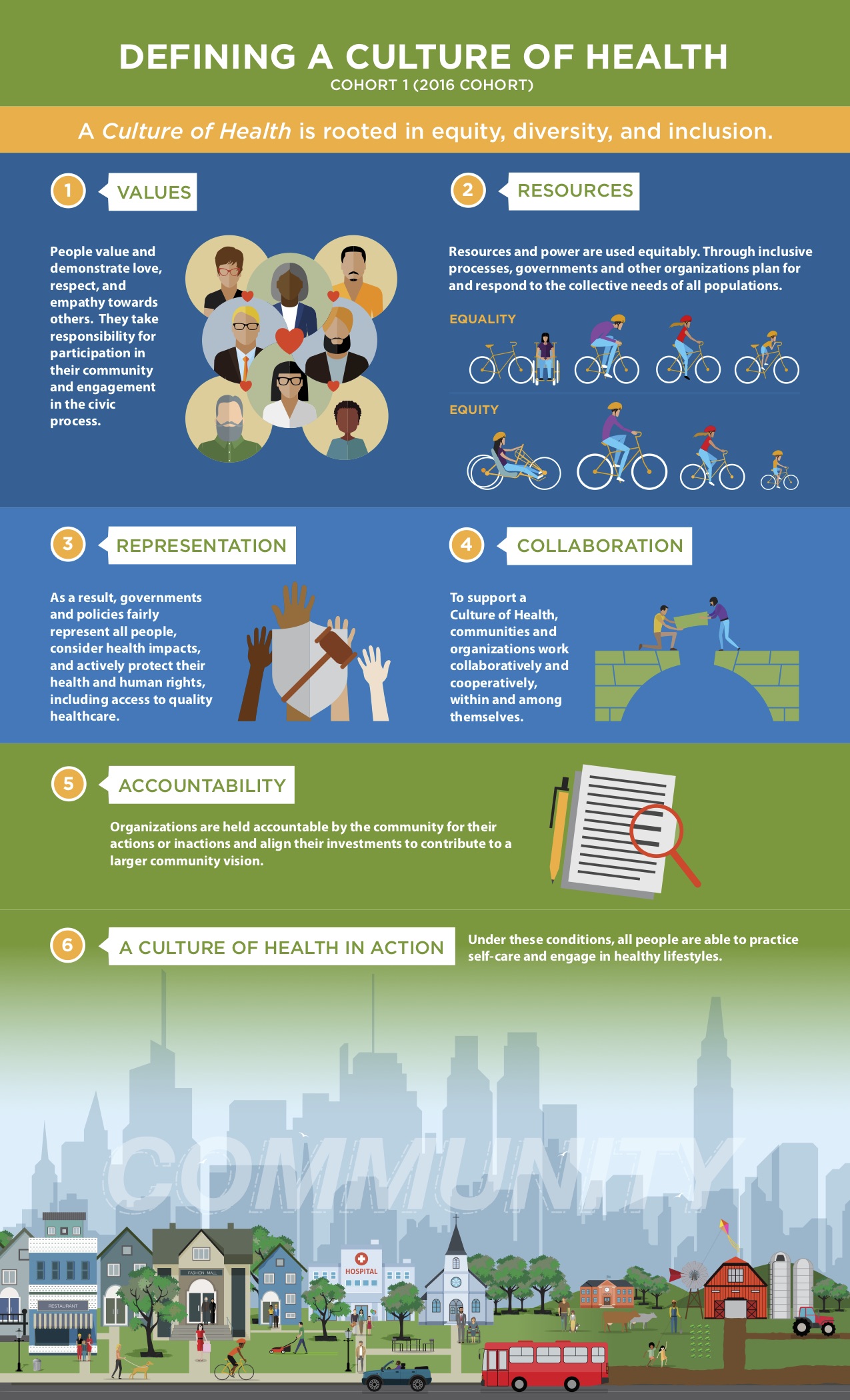
To sum all this up, we can achieve a healthier community by working together to create a culture where health is valued and we are all invested in helping one another achieve our best health and become our best selves. We can never be what we want to be as a community until we ALL have an opportunity to be as healthy and productive as we can be. We can do this together. We can build the community we want. We can build the future we want. But only if we build it together.